
Medicare Disproportionate Share Hospital (DSH) reimbursement has undergone numerous changes over the years, but it remains a material reimbursement stream for many hospitals.
Hospitals face both old and new challenges in preparing a complete, timely, and accurate data set for this decades-old program.
Below, we outline steps to help you seamlessly navigate a complete Medicare DSH process.
Ideal Medicare DSH Process
Whether you prepare Medicare DSH in house or outsource to a third party, the below cycle illustrates a best-practice approach for managing Medicare DSH from start to finish.
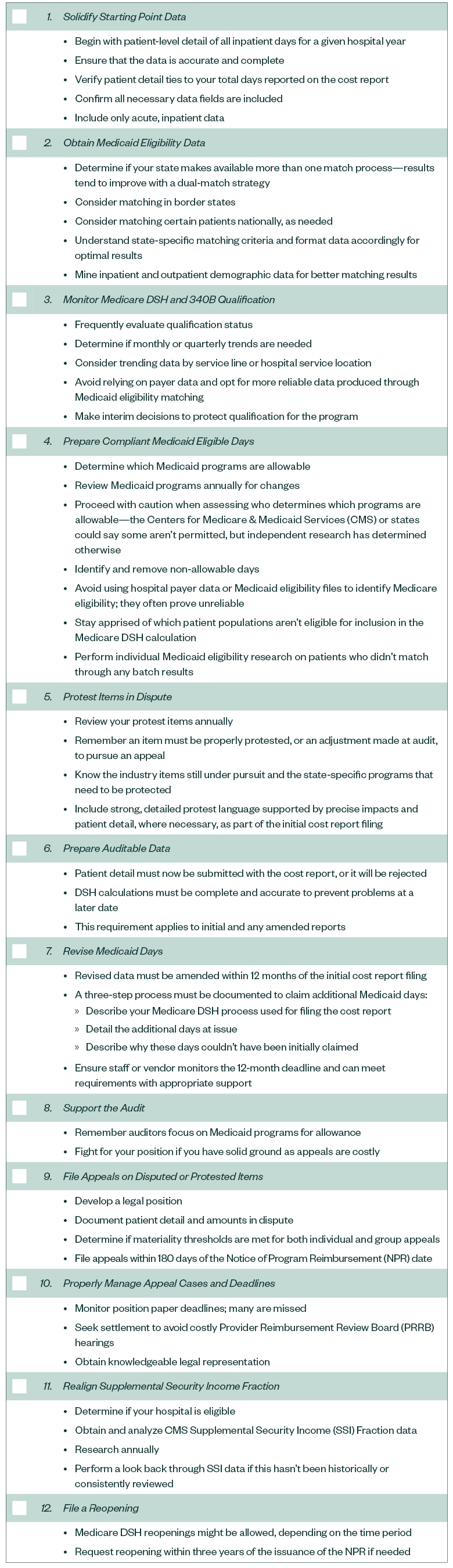
Medicare DSH Evaluation Checklist
The list below is a starting point for evaluating your Medicare DSH reporting program. You can also use our checklist to make sure your program is in order.
- Solidify Starting Point Data
- Obtain Medicaid Eligibility Data
- Monitor Medicare DSH and 340B Qualification
- Prepare Compliant Medicaid Eligible Days Listing
- Protest Items in Dispute
- Prepare Auditable Data
- Revise Medicaid Days
- Support the Audit
- File Appeals on Disputed or Protested Items
- Properly Manage Appeal Cases and Deadlines
- Realign Supplemental Security Income Fraction
- File a Reopening
There are many steps and state-specific issues not listed in the guidance that must be considered when preparing Medicare DSH calculations.
1. Solidify Starting Point Data
Patient-level detail of all inpatient days for a given hospital year should be used as the starting point to formulate the DSH calculation.
Before matching against state Medicaid roles, you should confirm data is accurate and complete. To be complete, your hospital’s data must:
- Tie to your total days reported on the cost report
- Contain all necessary data fields
- Include only acute, inpatient data
Many hospitals continue to over- or understate the inpatient data used to perform eligibility matches with the state compared to the cost report or total days work paper.
If your data is overstated, you risk creating compliance issues by including patients in the numerator of the DSH calculation that aren’t in the denominator.
If your data is understated, you risk potentially understating Medicare DSH by excluding patients from the numerator of the DSH calculation that are in the denominator.
Spending additional time and review efforts can help verify your starting point for Medicare DSH matching is correct.
2. Obtain Medicaid Eligibility Data
Once the starting point is confirmed to be accurate and complete, data should be matched against state Medicaid records.
Prior to matching:
- Determine if your state makes available more than one match process—results tend to improve with a dual-match strategy
- Consider matching in border states
- Consider matching certain patients nationally, as needed
- Understand state-specific matching criteria and format data accordingly for optimal results
- Mine inpatient and outpatient demographic data for better matching results
3. Monitor Medicare DSH and 340B Qualification
Hospital administration or pharmacy administration is requesting more frequent Medicare DSH updates to track 340B or Medicare DSH qualification status. To avoid year-end surprises:
- Determine if monthly or quarterly trends are needed
- Consider trending data by service line or hospital service location
- Avoid relying on payer data and opt for more reliable data produced through Medicaid eligibility matching
More timely data related to 340B and DSH qualification allows a hospital short of qualification or just barely meeting the threshold to make interim decisions to protect qualification for the program.
4. Prepare Compliant Medicaid Eligible Days Listing
Once Medicaid eligibility data is returned from the state, your hospital will need to compile a compliant Medicaid eligible days listing for the Medicare DSH calculation.
Your hospital will need to determine which Medicaid programs are allowable, who makes that decision, and how to identify and remove non-allowable days.
To do so, take the following steps:
- Review Medicaid programs annually for changes
- Proceed with caution when assessing who determines which programs are allowable—the Centers for Medicare & Medicaid Services (CMS) or states could say some aren’t permitted, but independent research has determined otherwise
- Avoid using hospital payer data or Medicaid eligibility files to identify Medicare eligibility; they often prove unreliable
- Stay apprised of which patient populations aren’t eligible for inclusion in the Medicare DSH calculation
Hospitals should also perform individual Medicaid eligibility research on patients who didn’t match through any batch results.
5. Protest Items in Dispute
If you haven’t reviewed your protest items recently or aren’t protesting any items, we recommend reviewing your processes. When protesting items, it’s important to:
- Remember an item must be properly protested, or an adjustment made at audit, to pursue an appeal
- Know the industry items still under pursuit and the state-specific programs that need to be protected
- Include strong, detailed protest language supported by precise impacts and patient detail, where necessary, as part of the initial cost report filing
6. Prepare Auditable Data
When filing cost reports for periods beginning on or after October 1, 2018, it’s important to remember the following:
- Patient detail must now be submitted with the cost report, or it will be rejected—this requirement applies to initial and any amended reports
- DSH calculations must be complete and accurate to prevent problems at a later date
7. Revise Medicaid Days
Many hospitals have material changes when retrospectively reviewing Medicaid eligible days. Revised data must be amended within 12 months of the initial cost report filing.
Additionally, a three-step process must be documented to claim additional Medicaid days:
- Describe your Medicare DSH process used for filing the cost report
- Detail the additional days at issue
- Describe why these days couldn’t have been initially claimed
This process will likely require exceptional documentation. It’s important your staff or vendor monitors the 12-month deadline and can meet these requirements with appropriate support.
8. Support the Audit
To support your audit, it’s important to remember that:
- Auditors focus on Medicaid programs for allowance
- Appeals are costly, so fight for your position if you have solid ground
9. File Appeals on Disputed or Protested Items
When filing appeals, your hospital must take steps to:
- Develop a legal position
- Document patient detail and amounts in dispute
- Determine if materiality thresholds are met for both individual and group appeals
- File appeals within 180 days of the Notice of Program Reimbursement (NPR) date
10. Properly Manage Appeal Cases and Deadlines
To organize appeal cases and meet deadlines, your hospital can:
- Monitor position paper deadlines; many are missed
- Seek settlement to avoid costly Provider Reimbursement Review Board (PRRB) hearings
- Obtain knowledgeable legal representation
11. Realign Supplemental Security Income Fraction
This process only applies to hospitals with a fiscal year-end that isn’t September 30.
CMS Supplemental Security Income (SSI) Fraction data must be obtained and analyzed to prevent a downside and to calculate the upside, by year.
Hospitals should research annually whether their facility could benefit from realigning their SSI percentage. If this hasn’t been historically or consistently reviewed, your hospital should perform a look back through its SSI data.
12. File a Reopening
Medicare DSH reopenings might be allowed, depending on the time period.
If a reopening is needed, it must be requested within three years of the issuance of the NPR.
Proactive Planning
The Medicare DSH calculation is a complex program, with many tripping points.
Maintaining compliance while achieving optimization requires diligent effort and pristine record keeping. There are no shortcuts to achieving this goal.
Medicare DSH Evaluation Checklist
There are also many steps and state-specific issues not listed in the guidance that must be considered when preparing Medicare DSH calculations.
We’re Here to Help
To learn about what Medicare DSH opportunities might exist for your hospital, request a complimentary analysis report or contact your Moss Adams professional.